As children, most of us sat through health class where we learned the basics of reproduction. We were taught how to avoid pregnancy, abstinence, condoms or other forms of protection, which is information we dutifully used into our 20’s or later. So, when the time comes to begin building a family, many of us find ourselves wanting for information. We spend so many years working to prevent pregnancy that some of us do not consider the ins and outs of family building until it is too late.
Definition of Infertility
For years I have been encouraging couples to see a specialist if they have been struggling to have a baby for one year (if the woman is under age 35) or six months (age 35 or older). For most patients, this guideline is helpful. There is a wide range of assisted reproductive technologies (ART) that can – and often do – help couples. If nothing else, the guideline gives patients a sense of the time that it typically takes patients to have a baby. At 35, women have a 15 to 20 percent chance of getting pregnant in any given month, and this number drops significantly for women over 35.
However, this guideline is only part of the picture. It’s important that women understand that they should not wait until they are ready to have a baby to be informed about their fertility.
Be Proactive
Our choice to have a family does not begin after we get married; most of us start dreaming of what it will be like to have a family of our own as young children. To preserve our reproductive health, there are several choices we can make as early as our teens.
One of the most empowering things a woman or a man can do is to learn more about their personal reproductive health. Regardless if a woman is 17 or 47, and ready to have a baby now or decades away, she needs annual OB/GYN appointments. Women should start checking their fertility and reproductive health in their 20’s. This includes a physical exam and blood tests, such as follicle stimulating hormone (FSH) and anti-mullerian hormone (AMH). If an OB/GYN does not routinely conduct such tests, ask for it.
Lifestyle habits such as nutrition, exercise and sleep patterns are all factors in our reproductive health. A diet full of fruits, vegetables, whole grains, lean protein and healthy fats is the foundation for good health that affects every aspect of our body’s function. Throw in regular exercise and a full night’s restorative rest, and you are off to a good start.
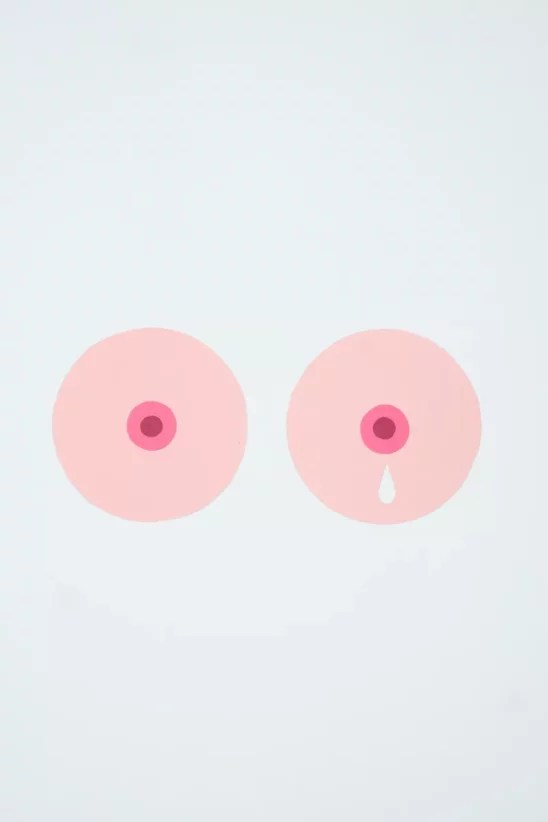
It’s also important to avoid excessive use of common vices such as caffeine, alcohol and smoking (tobacco and marijuana), all of which can have a negative effect on oocytes and sperm. It’s wise to never start smoking cigarettes (or at least quit immediately). Cigarettes have more than 4,000 chemical compounds, including 43 carcinogens or poisons that contribute to miscarriage, diminished quality in oocytes and sperm, male infertility and sexual dysfunction.
Special Circumstances
Certain patients with unique medical needs or chronic conditions may opt to see a Reproductive Endocrinology and Infertility specialist (REI) earlier in their reproductive journey.
It is also of utmost importance that oncology patients have a consultation with an REI. Chemotherapy and radiation, while lifesaving, can damage patients’ sperm and eggs. Patients do not have to choose between cancer treatment and having a family. Fertility preservation does not significantly delay cancer treatment. It can be done within a day for men and within two weeks for women. This is done in conjunction with a patient’s cancer schedule with the blessings of their oncologist.
When You’re Ready to Make an Appointment
Women who are curious about their fertility or have concerns may be hesitant to make an appointment with a fertility specialist. Your first visit as a new patient generally involves a review of your medical history and the offer of any testing that may help you toward your family building goal.
Some patients have not started to try for a family, and just want information. Others may have been trying for some time. In addition, REI’s see many types of patients that are single parents-to-be, same sex relationships, or patients who are not ready for families but want to preserve their fertility. An REI role is to give patients all the support they need alongside advanced medical treatment.
Usually the next step is a diagnostic work-up. For women, this includes a physical exam, blood work and an ultrasound. For men, diagnostic testing includes checking a sperm count, which includes motility (how it moves) and morphology (shape) analysis.
Moving Forward
Part of building a relationship with an REI doctor is meeting your whole care team that can include your nurse, financial advocate, nutritionist, acupuncturist and reproductive coaching staff. What is most important is seeing you succeed at your dream of having a family.
Spencer Richlin, M.D. is Surgical Director and a Fertility Specialist in reproductive endocrinology at Reproductive Medicine Associates of Connecticut (RMACT), as well as Chief of Reproductive Endocrinology and Infertility (REI) in the Department of Obstetrics and Gynecology at Norwalk Hospital. He is Board Certified in both Reproductive Endocrinology & Infertility and Obstetrics and Gynecology. rmact.com.