Q: What should parents know about childhood urinary incontinence?
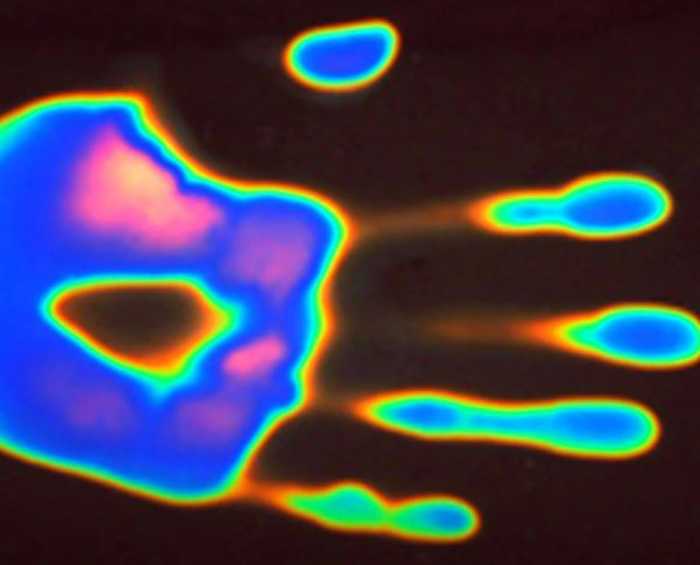
When an infant’s bladder fills a built-in reflex is triggered and the bladder empties resulting in a wet diaper. As the baby ages the frontal lobes of its brain mature, enabling the child to suppress this reflex so urine can be contained in the bladder.
It’s important to note that the occasional, involuntary loss of urine is common until the age of 5. If incontinence persists past this age parents should seek counsel from their child’s pediatrician, who may refer them to a specialist such as a pediatric urologist.
Q: Are there different types of incontinence?
Yes, and they are subdivided into daytime and nighttime categories. Daytime issues are separated into physical/neurological and functional problems. And while daytime functional and nighttime incontinence are different issues, both are related to a child’s inability to suppress the bladder-emptying reflex.
Q: What are the causes?
Constipation can lead to both daytime and nighttime incontinence and tackling this issue should be the first course of action taken.
Daytime incontinence often suggests a ‘functional’ problem rather than a physical one, and is commonly associated with immaturity in the brain that controls urination.
However, certain forms of daytime incontinence can also indicate a physical problem, but these instances are usually rare. The physical problem can also lead to renal damage which can be associated with excessive urine production.
Nighttime incontinence is almost never a physical problem. It is generally related to the brain not being able to suppress reflexes to urinate while the child is sleeping. In some patients this is due to inadequate production of a hormone that reduces urine production at night.
There is also a high association between nighttime wetting and attention deficit disorder and some other neuropsychiatric problems.
Q: Can a child grow out of it?
If a child’s urinary incontinence is not due to a physical issue then the majority of children will grow out of the problem if the child is still wetting by age 10 there is a 33% chance they can have problems as adults and intervention is recommended.
Also, studies show that if one parent experienced nighttime wetting his or her child has a 50 percent chance of having a similar problem. If both parents had nighttime wetting issues their son or daughter has a 70 percent chance of having the same issue.
Q: What are the treatments?
First and foremost address any constipation issues. The rectum is adjacent to the bladder and the brain and spine can confuse rectal contractions with bladder contractions.
For daytime incontinence simple therapies can be attempted, such as having the child void five times a day, managing fluid intake and diet. An ultrasound of the bladder and kidneys is also necessary. In some cases, children will benefit from biofeedback treatment. Medications are a last resort.
If nighttime incontinence is an issue, families can try a conditioning alarm system, which has a 70% efficacy rate.
Be aware the alarm wakes the child after he or she wets, not before. To be effective everyone has to be invested in this process. The alarm system must be used consistently for at least three months as conditioning takes time to develop. Consistent application far outweighs the type and cost of the alarm system.
Other tips for nighttime incontinence include ensuring your child urinates before bed and eliminating dairy products after dinner.
You may also want to wake your child within one or two hours of sleep and take him or her to the bathroom as most urine is made during the first few hours of rest.
And some children may just generate more urine than others. With these cases medication can be used and there is a 50-70 percent success rate.
REMEMBER …
Parents must never admonish, embarrass or punish a child for daytime or nighttime incontinence. Punishing will never help and can even make the problem worse as the child doubles his or her efforts to ‘hold’ urine. This can lead to voiding problems, which can have profound effects on the bladder and, in rare cases, lead to renal failure.
Israel Franco, M.D., is Director of Pediatric Urology at Maria Fareri Children’s Hospital at Westchester Medical Center, the children’s hospital for Westchester County, the Hudson Valley and Fairfield County. 877-WMC-DOCS (877-962-3627). westchestermedicalcenter.com/mfch.